Epilepsy Surgery Treatment
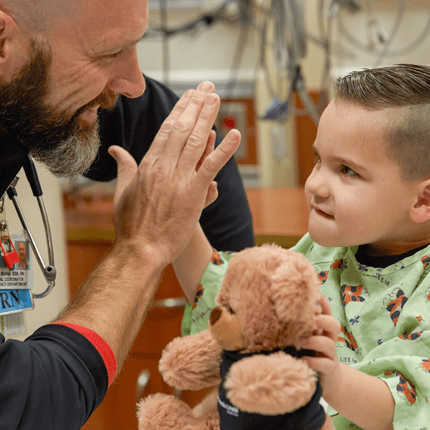
Children with medically uncontrolled seizures can be evaluated and considered for the Epilepsy Surgery Program at the Children’s Hospital of Michigan.
The Epilepsy Surgery Program at the Children’s Hospital of Michigan exists to serve children with difficult to manage or uncontrollable seizures. Since its inception in 1994, pediatric patients from Michigan and throughout the world have benefitted from the highly specialized diagnostic and treatment techniques used at the Children’s Hospital of Michigan. Below is a summary of epilepsy surgical procedures used at the Children’s Hospital of Michigan.
Hemispherectomy
In some cases, the seizures are initiated from the entire non-functioning hemisphere of the brain. Some causes of these seizures include malformations of the cortex, strokes that happen before and after birth, Sturge Weber Syndrome and Rasmussen’s Encephalitis. In patients with these conditions, pediatric neurosurgeons can disconnect or remove the non-functioning hemisphere in a surgical procedure called hemispherectomy, which can give the child complete freedom from seizures. If the side of the child’s body opposite the affected hemisphere is already weak or has paralysis, this may continue after the surgery is performed.
For the past eight years, Sandeep Sood, MD, a pediatric neurosurgeon on staff at the Children’s Hospital of Michigan, has pioneered the development of endoscopic minimally invasive surgery for hemispherectomy. Dr. Sood uses a 3D endoscope with an incision only an inch in length, minimizing blood loss, and thus lowering the risks involved in brain surgery. Minimally invasive surgery is intended to result in a shorter hospital stay. Candidates for this procedure must have their seizures arise from a specific part of the brain, and undergo exhaustive testing to determine that this part of the brain can be safely removed with minimal or no consequences for the child. The goal of hemispherectomy is to remove the seizure focus while preserving the child’s functionality and improve the quality of life for the child and his/her family.
Focal Cortical Resection
When a specific area or location of the brain is found to be the reason for seizures, doctors may perform a Focal Cortical Resection or “Lobectomy,” which may involve the temporal, frontal, parietal or occipital lobes of the brain. Abnormal
tissue in the brain, identified in testing as tumors, brain malformation or blood vessel malformation, can be a focal area of seizure onset. Surgeons may use brain-mapping tools to best identify the seizure focus.

MRI Guided Laser Interstitial Thermal Ablation Therapy - Minimally Invasive Brain Surgery For Epilepsy and Brain Tumors
Laser Interstitial Thermal Ablation Therapy (LITT) is a minimally invasive neurosurgical technique surgery using a fiber optic laser to destroy seizure-producing brain tissue and brain tumors through a small, ¼ inch, scalp incision. The laser heats and destroys the area of abnormal brain tissue, as real-time MRI images monitor the procedure. MRI-guided laser ablation offers a high level of precision and control, providing an alternative to conventional open surgical procedures.
Multiple Subpial Transections
Multiple Subpial Transections (MST) can be performed in a one-stage surgery or part of a two-stage surgery, where a resection is performed. But removing certain areas of the cortex is not optimal, such as the motor or language cortex which can affect speech. This surgery also is used in patients with Landau Kleffner, Rasmussen’s Encephalitis and brain malformations. During MST surgery, parallel cuts are made through the cortex and perpendicular to the gyrus of the brain. The idea is that cross-cut nerve fibers that run horizontal along the cortex limit the spread of the electrical seizure discharge. This procedure may reduce the number of seizures but will not eliminate them completely.
Corpus Callosotomy Surgery
For children with intractable drop seizures – seizures that cause the child to suddenly lose muscle tone, nod their heads, drop things and fall to the ground – a palliative procedure called corpus callosotomy, may help lessen the seizure burden.
Click here to learn more about this procedure.
Vagus Nerve Stimulator Implant
For children with uncontrolled seizures without resectable seizure focus, a vagus nerve stimulator (VNS) may be a viable treatment alternative. The VNS is implanted under the chest wall and contains a wire that runs from it to the vagus nerve in the neck. VNS therapy delivers frequent mild electrical pulsations to the brain’s vagus nerve, similar to that of a pacemaker. Once implanted, the device, about the size of a silver dollar, is programmed to deliver customized impulses based upon the patient’s unique needs. For patients who anticipate their seizures and know when they will happen, they can hold a special magnet near the implant which can trigger it to deliver a pulse outside of its normal programming. Doing so can help abort their seizures, and/or shorten their duration.